Abstract
BACKGROUND: Despite mounting knowledge, the management of patients with acute myeloid leukemia (AML) can be challenging, particularly for relapsed/refractory patients who lack innovative, effective treatments. Recent preclinical studies of AML have demonstrated promissory therapeutic activity of the novel class of inhibitors of bromodomain and extra terminal (BET) family proteins. To identify AML patients that may benefit from BET inhibitor treatment, we sought to discover and evaluate predictive molecular biomarkers for sensitivity towards BET inhibition, focusing on the prototype BET inhibitor JQ1.
METHODS: Following written informed consent and according to the Declaration of Helsinki, bone marrow, peripheral blood, and skin biopsy samples were obtained prospectively from AML patients (n=139) and analyzed for their whole exome profiles and ex vivo responses to JQ1 exposure, as part of an Individualized Systems Medicine (ISM) study of AML (Pemovska et al., 2013). Consequently, associations between molecular features and drug responses were investigated using logistic regression models for data integration. Novel signals emerging from our cohort of patients were carried forward for reproducibility assessment in publicly available cell line datasets (Cancer Cell Line Encyclopedia and Catalogue of Somatic Mutations in Cancer for genomic data, and Cancer Therapeutics Response Portal and Genomics of Drug Sensitivity in Cancer for drug response data). In addition, literature-reported indicators of sensitivity were examined in the AML cohort in order to evaluate their clinical translatability.
RESULTS: Enabling a genome-wide search for predictive biomarkers for BET inhibitor response, our bioinformatics pipeline returned a set of signals significantly associated with JQ1 treatment.
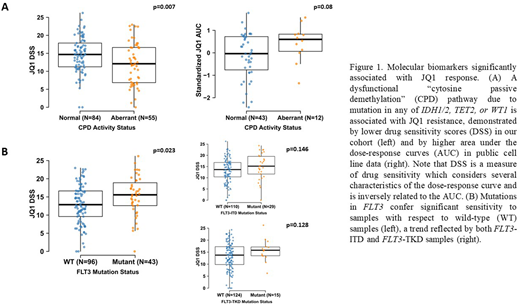
Frequently mutated in AML, isocitrate dehydrogenases IDH1 and IDH2, tet methylcytosine dioxygenase TET2, and Wilms' tumor WT1 each appeared to confer resistance upon mutation to the samples harboring them. Participating in a common biochemical pathway, the 4 genes have been shown to be mutated following a mutual exclusivity pattern in AML (Scourzic et al., 2015), which was successfully replicated in our cohort. Accordingly, grouping of samples with mutation in any of the genes yielded a significantly more resistant group to JQ1 treatment in comparison to wild-type samples. Incorporation of TET2 and WT1 deletions from the samples' copy number variation data supported this hypothesis. Importantly, this observation was also successfully validated in cell line drug sensitivity data (Figure 1A).
Moreover, FLT3-mutated samples in our cohort returned significantly higher sensitivity scores to JQ1 compared to wild-type samples, irrespective of their NPM1 mutation status. The superior response trend observed within this group was maintained independently of whether the mutation was an internal tandem duplication (FLT3-ITD) or in the tyrosine kinase domain (FLT3-TKD) of the gene (Figure 1B).
Finally, and in contrast to other studies, AML samples harboring mutation to NPM1 were not significantly more sensitive to BET inhibition with respect to NPM1 wild-type samples.
CONCLUSION: Taken together, the results suggest novel insights for the stratification of AML patients for treatment using BET inhibition therapy, taking this malignancy's heterogeneity into account. Particularly, while FLT3 mutations are to be considered as sensitizing factors to BET inhibitors, samples with mutations in IDH1, IDH2, TET2, or WT1 were resistant, and thus, patients harboring these gene mutations may not benefit. These observations also propose drug partners that are worth investigating in combination with BET inhibitors in the defined patient subpopulations, namely FLT3 inhibitors and hypomethylating agents (or IDH1/2 inhibitors), respectively. Furthermore, the variability of responses observed among samples harboring NPM1 mutations highlights the molecular heterogeneity existing within this group of patients, stressing the need for identifying additional companion diagnostics for a more effective stratification of this population. Although our findings require additional validation in a larger cohort and through clinical investigations, this study provides evidence of molecular indicators that could help identify AML patients that would benefit from BET inhibitor therapy.
Tsallos:Novartis: Research Funding. Wennerberg:Novartis: Research Funding. Porkka:Celgene: Honoraria, Research Funding; Novartis: Honoraria, Research Funding. Heckman:Novartis: Research Funding; Orion Pharma: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal